What You Need to Know About Addiction Right Now
Addiction is a chronic, relapsing brain disorder characterized by compulsive drug seeking and use despite harmful consequences. Here’s what you need to understand:
- It’s a Disease, Not a Choice – Addiction fundamentally changes brain circuits involved in reward, stress, and self-control.
- Recovery is Possible – With proper treatment and support, people can and do recover from addiction.
- It Affects Everyone – According to 2025 data, about 10% of people aged 12 or older in the U.S. have alcohol use disorder alone.
- Multiple Forms Exist – Addiction includes both substance addictions (drugs, alcohol) and behavioral addictions (gambling, internet use).
- Genetics Play a Role – 40-60% of addiction risk comes from genetic factors.
- Early Use Increases Risk – Over 90% of people with addiction began using before age 18.
Addiction doesn’t discriminate, impacting people from all walks of life. In 2025, substance use disorders affect millions of Americans, with drug overdoses claiming over 63,000 lives.
The good news is that addiction is treatable. Like other chronic conditions such as diabetes or heart disease, it can be managed successfully with proper care.
If you or a loved one is struggling, you’re not alone. Recovery begins with understanding addiction and recognizing that seeking help is a sign of strength.
At Drug Rehab Headquarters, we support individuals and families with compassionate, evidence-based care. Our specialists understand that each recovery journey is unique and are here to help you find treatment options custom to your needs.
If you or a loved one needs help today, call 866-720-3784 for a free, confidential consultation.

Understanding Addiction: Definitions, Types, and Brain Science
Addiction is a complex neuropsychological disorder defined by a persistent urge to use a substance or engage in a behavior, despite substantial harm. It’s not a moral failing but a chronic, relapsing disorder that fundamentally changes the brain. This medical illness involves compulsive use despite negative outcomes, and these brain changes can be long-lasting.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), uses the term “Substance Use Disorder” (SUD) to describe this condition on a spectrum from mild to severe. The DSM-5 criteria for SUD fall into four main categories:
- Impaired Control: Using more of a substance than intended, wanting to cut down but being unable to, spending significant time on use, and experiencing cravings.
- Social Impairment: Neglecting responsibilities at work, school, or home; continuing use despite social problems; and giving up important activities.
- Risky Use: Using substances in risky situations and continuing use despite knowing it causes physical or psychological problems.
- Pharmacological Criteria: Developing tolerance (needing more for the same effect) and experiencing withdrawal symptoms when stopping use.
At its core, addiction is a disorder of the brain’s reward system. Addictive drugs and behaviors flood this system with dopamine, a neurotransmitter that reinforces rewarding behaviors. This overstimulation creates a powerful learning signal, making it hard to stop. Over time, this alters brain circuits involved in reward, stress, and self-control, perpetuating cravings and weakening self-control. You can learn more through scientific research on the brain disease model of addiction.
The Brain Disease Model of Addiction
The American Society of Addiction Medicine (ASAM) defines addiction as a chronic brain disorder. This model frames addiction as a medical condition, not a moral failing. While initial use may be voluntary, continued use changes the brain’s structure and function, impairing judgment and hijacking reward pathways, making substance use feel like a necessity.
Viewing addiction as a brain disease reduces stigma, shifting the focus from “bad choices” to “biological changes” and fostering compassion. While choice plays a role, genetics account for 40-60% of a person’s risk, creating a biological predisposition for many. Recognizing this allows for more empathetic care.
Categories of Addiction: Substance and Behavioral
Addiction is categorized into two main types: substance and behavioral. Both involve compulsive engagement despite negative consequences and can significantly impair a person’s life.
Substance Addictions (Substance Use Disorders): These involve the compulsive use of psychoactive substances.
- Alcohol Use Disorder: The most common substance addiction in the U.S., affecting about 10% of people aged 12 or older, according to 2025 data.
- Opioid Addiction: Includes illicit drugs like heroin and prescription painkillers like fentanyl.
- Stimulant Addiction: Involves methamphetamine, cocaine, and prescription stimulants like Adderall.
- Nicotine Addiction: A widespread addiction, primarily through tobacco, often starting in adolescence.
- Cannabis Addiction: Can lead to dependence and withdrawal, especially with high-strength varieties.
- Other Substance Addictions: Includes hallucinogens, sedatives, inhalants, and more, each with unique risks.
Behavioral Addictions (Non-Substance Addictions): These involve compulsive engagement in rewarding activities. While only gambling disorder is formally recognized in the DSM-5, others are widely studied.
- Gambling Disorder: A formally recognized disorder involving persistent, problematic gambling.
- Internet Gaming Disorder: Listed in the DSM-5 for further study, it involves compulsive online gaming.
- Food Addiction: Compulsive overeating of highly palatable foods despite negative health effects.
- Other Potentially Addictive Activities: Includes shopping, sex, pornography, and excessive internet use.
Here’s a quick list of some common addictions:
- Substance Addictions:
- Alcohol
- Opioids (Heroin, Fentanyl)
- Stimulants (Cocaine, Methamphetamine)
- Nicotine
- Cannabis
- Benzodiazepines
- Behavioral Addictions:
- Gambling
- Internet Gaming
- Food
- Sex
- Shopping
The Path to Addiction: Causes and Key Risk Factors
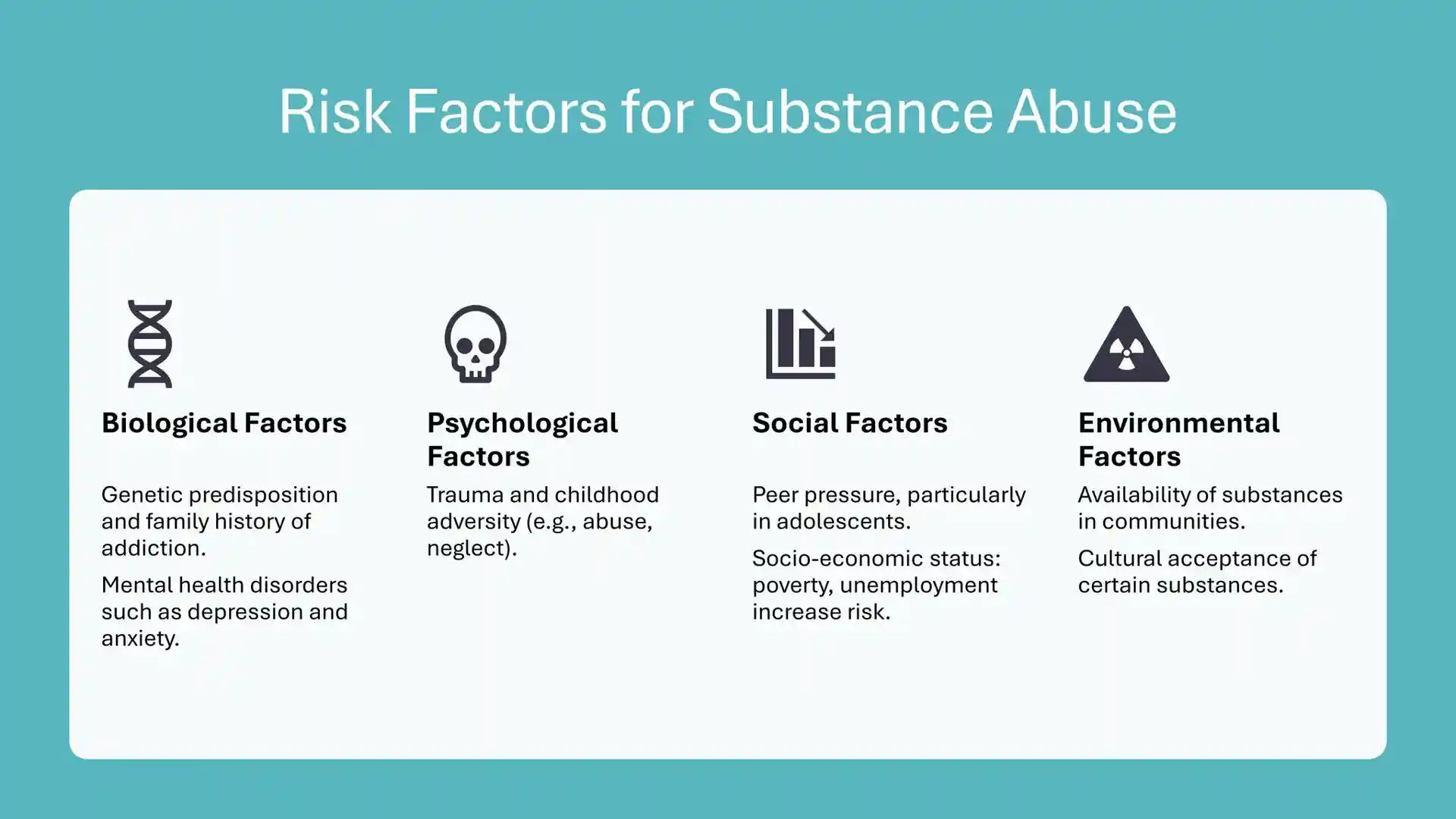
No one plans to become addicted. Addiction develops from a complex mix of genetic, environmental, and developmental factors. Understanding these helps in prevention and intervention.
Why People Start Using Substances
People begin using substances for various reasons, often seeking a temporary change in their state of being.
- Experimentation and Curiosity: Common among adolescents, leading to initial drug use.
- Social Influence: Peer pressure is a major factor, especially for youth. Over 90% of people with an addiction started using before age 18.
- To Feel Good: Substances can produce a powerful, motivating “high” by creating euphoria.
- To Feel Better (Self-Medication): Substances are often used to cope with anxiety, depression, or trauma. According to 2025 data, over 50% of people with SUDs also have co-occurring mental health issues.
- To Do Better: Some use substances to improve academic, professional, or athletic performance.
- Coping Mechanism: Substances can offer a temporary escape from difficult emotions or chronic pain.
- Novelty Seeking: This personality trait can predispose individuals to trying drugs.
Factors That Increase the Risk of an Addiction
While initial use is voluntary, certain factors increase vulnerability to developing an addiction.
- Genetic Predisposition: Genes account for 40-60% of a person’s addiction risk. A family history of addiction increases susceptibility.
- Family History: A home environment with substance use, lack of parental supervision, or chaos increases risk.
- Early Exposure and Age of First Use: Starting drug use as an adolescent is a major risk factor. The developing brain is more vulnerable to long-lasting changes from substance use. Over 90% of people with addiction started before age 18.
- Environmental Factors: Drug availability, peer influence, poor social skills, and community poverty all increase risk.
- Trauma and Stress (Adverse Childhood Experiences – ACEs): Childhood trauma, abuse, or chronic stress significantly increases addiction vulnerability, often leading to self-medication.
- Co-occurring Mental Health Disorders: Conditions like depression, anxiety, or PTSD increase the risk of using substances to cope, complicating treatment.
- Personality Traits: Impulsivity and sensation-seeking are linked to higher addiction risk.
- Method of Drug Administration: Smoking or injecting drugs increases addictive potential due to the rapid, intense high.
Conversely, protective factors like strong family bonds, parental involvement, and academic success reduce risk. Building resilience and developing healthy coping mechanisms are vital. You can find more info about risk factors from the National Institute on Drug Abuse.
Recognizing the Signs and Finding Treatment
Recognizing the signs of addiction is the first step toward getting help. It’s often challenging because people may hide their struggles or be in denial. Knowing the common indicators can help you identify when someone needs support.
Common Signs and Symptoms of Addiction
The signs of addiction can be behavioral, physical, and psychological.
Behavioral Changes:
- Neglecting Responsibilities: Failing to meet obligations at work, school, or home.
- Changes in Routine: Spending excessive time obtaining, using, or recovering from the substance.
- Risky Behaviors: Engaging in hazardous activities like driving while impaired.
- Social Withdrawal: Isolating from family, friends, and hobbies.
- Continuing Use Despite Harm: Using despite negative physical, psychological, or social consequences.
- Failed Attempts to Stop: Wanting to quit or cut down but being unable to.
- Financial Strain: Unexplained money problems or stealing to support the habit.
Physical Symptoms:
- Changes in Appearance: Neglected hygiene, weight changes, or track marks.
- Increased Tolerance: Needing more of the substance for the same effect.
- Withdrawal Symptoms: Physical and psychological distress when not using (e.g., nausea, anxiety, tremors).
- Changes in Sleep Patterns: Insomnia or sleeping too much.
- Pupil Changes: Dilated or constricted pupils.
Psychological Signs:
- Intense Cravings: A powerful urge to use.
- Mood Swings: Unexplained mood shifts, irritability, or agitation.
- Denial: Minimizing or denying the problem’s severity.
- Distorted Thinking: Rationalizing use or blaming others.
- Loss of Control: Inability to limit use.
If you see these signs, it’s crucial to seek professional help. Recovery is possible with the right support. For more detailed information, consult resources like the Mayo Clinic’s guide on drug addiction symptoms.
Evidence-Based Treatment Approaches
Effective addiction treatment is personalized, addressing an individual’s unique needs. At Drug Rehab Headquarters, our approach uses evidence-based practices for lasting recovery.
- Detoxification (Detox): Often the first step, medically assisted detox safely manages withdrawal symptoms. It must be followed by further treatment for long-term recovery.
- Inpatient vs. Outpatient Care: Inpatient/Residential treatment offers a structured, 24/7 environment, ideal for severe cases. Outpatient treatment allows individuals to live at home while attending regular therapy sessions.
- Behavioral Therapies: These are cornerstones of treatment, helping modify problematic thoughts and behaviors.
- Cognitive Behavioral Therapy (CBT): Teaches coping skills to avoid triggers.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation and is useful for co-occurring disorders.
- Motivational Improvement Therapy (MET): Helps resolve ambivalence about treatment.
- The Matrix Model: A structured approach for stimulant addiction.
- Family Behavior Therapy (FBT): Involves family to address dynamics contributing to substance use.
- 12-Step Facilitation Therapy: Encourages participation in support groups like AA or NA.
- Medication-Assisted Treatment (MAT): For many substance addictions, combining therapy with medication is most effective.
- Opioid Use Disorder: Methadone, buprenorphine, and naltrexone reduce cravings and withdrawal.
- Alcohol Use Disorder: Naltrexone, acamprosate, and disulfiram help reduce drinking and manage cravings.
- Nicotine Addiction: Nicotine Replacement Therapies (NRTs) and other medications aid in quitting smoking.
- Dual Diagnosis Treatment: Integrated treatment addresses both addiction and co-occurring mental health disorders simultaneously for better outcomes.
- Aftercare and Support Groups: Lifelong recovery involves aftercare, ongoing therapy, and support groups (AA, NA) for continued support and relapse prevention.
At Drug Rehab Headquarters, we understand addiction treatment across the country, including states like Alabama, California, Florida, and Texas. We connect you with the right resources to start your healing journey. If you’re ready to find treatment options, we can guide you.
Frequently Asked Questions About Addiction
We encounter many questions about addiction, and we believe that clear, accurate information is vital for understanding and addressing this complex health issue.
What is the most common type of addiction?
In the U.S., the most common substance addiction is Alcohol Use Disorder. 2025 statistics show it affects about 10% of people aged 12 or older. Nicotine and marijuana use disorders are also prevalent. The accessibility and social acceptance of alcohol and tobacco contribute to high addiction rates. While cannabis is more accepted, its addictive potential is a growing concern.
Can addiction be cured?
Addiction is a chronic disease like diabetes, meaning it can be managed but not “cured.” Recovery is about achieving remission, where symptoms are controlled. It’s a lifelong process of management and support. Relapse is a part of this process and indicates a need to adjust treatment, not that it has failed. With consistent effort, long-term recovery from addiction is achievable.
How can I help a loved one with an addiction?
Helping a loved one with addiction is challenging. You can’t “fix” them, but you can encourage them to seek help and support their recovery.
Here are some ways you can help:
- Educate Yourself: Learn about addiction as a disease to approach the situation with empathy.
- Express Concern: Talk to your loved one about your concerns, focusing on specific behaviors and their impact without being accusatory.
- Avoid Enabling: Don’t protect them from the consequences of their actions (e.g., giving money, making excuses), as this can perpetuate the addiction.
- Set Healthy Boundaries: Establish clear boundaries to protect your own well-being.
- Encourage Professional Help: Firmly encourage them to seek treatment and offer to help them find it.
- Seek Support for Yourself: Find support through groups like Al-Anon or family therapy to manage your own stress.
- Consult a Professional: A professional intervention can be an effective way to motivate a loved one to seek treatment.
It’s a balance of support and boundaries. If you’re unsure how to proceed, professional guidance is a powerful step. The team at Drug Rehab Headquarters can offer family support resources. Call 866-720-3784 for family support resources.
Conclusion: A Future Free from Addiction
We’ve seen that addiction is a complex medical condition, not a choice, influenced by genetics, environment, and mental health. The journey to recovery is challenging but achievable. Through evidence-based treatment and ongoing support, people can regain control of their lives and build a future free from the grip of addiction. The biggest barrier is often stigma, which prevents many from seeking the help they need.
At Drug Rehab Headquarters, we work to make hope and healing accessible by breaking down these barriers and connecting people with quality care. Recovery is a reality for millions nationwide, from New York to California.
Taking the first step is the most courageous act. Our team is here to guide you with compassion and help you find support custom to your needs. We can help you explore top-rated rehabs in states like Nevada, California, Florida, Georgia, and many others where we have vetted high-quality facilities.
Don’t let addiction define your future. You can start exploring options today and explore top-rated rehabs in Nevada to begin your journey to lasting recovery.

