The Critical Reality of Adolescent Substance Abuse Health Risks
Adolescent substance abuse health risks are far more serious than many parents realize. Here’s what every parent needs to know:
Key Health Risks:
- Brain Damage: Can permanently alter brain development, affecting memory, decision-making, and learning.
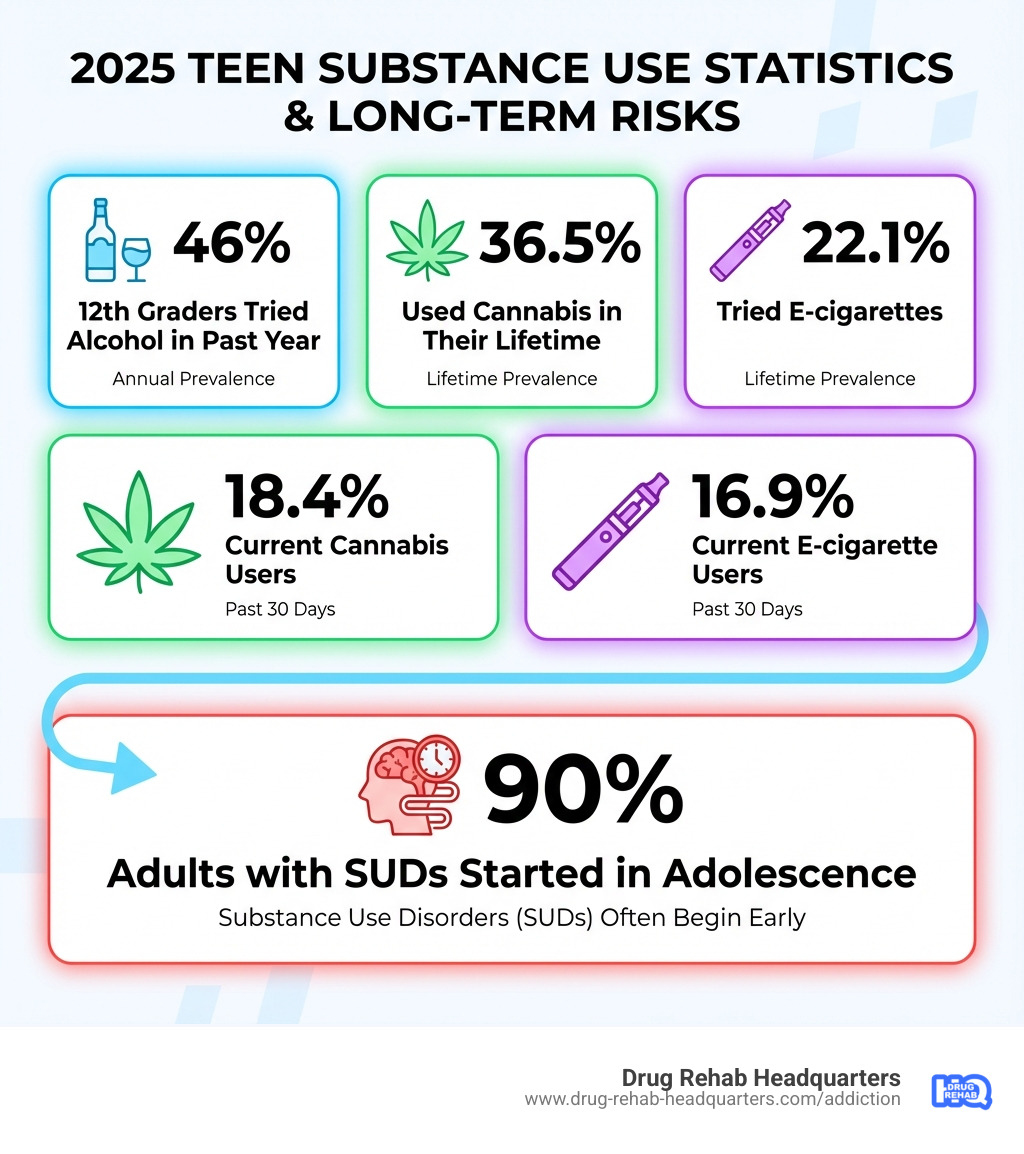
- Addiction: Over 90% of adults with substance use disorders began using as teens.
- Mental Health Issues: Substance use is strongly linked to depression, anxiety, and other disorders.
- Injury and Death: A leading factor in unintentional injuries, suicide, and violence among teens.
- Fatal Overdose: The risk is heightened by fentanyl contaminating the drug supply.
- Poor Life Outcomes: Increases lifetime risk of chronic disease, legal issues, and poor educational/career results.
The numbers paint a sobering picture. Projections for 2025 show that 46% of 12th graders will have tried alcohol in the past year, 18.4% will be current cannabis users, and 16.9% will be current e-cigarette users. These trends underscore the urgency for awareness and intervention.
At Drug Rehab Headquarters, we’ve dedicated our work to helping families understand and address adolescent substance abuse health risks through compassionate, confidential support and evidence-based treatment connections. We know that early intervention saves lives, and we’re here to guide you through every step of the recovery journey—call us anytime at 866-720-3784 for free, confidential help.
Handy adolescent substance abuse health risks terms:
The Developing Teen Brain: Why Adolescence is a High-Risk Period

Adolescence is a time of incredible growth, not just physically, but neurologically. While teenagers might look like mini-adults, their brains are still under construction, a process that can extend to age 25 and makes this a high-risk period for substance use.
The teen brain develops unevenly. The prefrontal cortex, responsible for judgment and impulse control, matures last. In contrast, the limbic system, which governs emotion and reward, develops earlier. This imbalance makes teens naturally prone to reward-seeking and emotional responses while their ability to weigh risks is still catching up.
This dynamic is amplified by the brain’s highly sensitive pleasure circuit (the mesolimbic dopamine system). During adolescence, substances can produce a more intense “high,” quickly leading to dependence. This heightened reward sensitivity, combined with an immature prefrontal cortex, makes teens more prone to risky behaviors like substance use.
Beyond biology, social and emotional factors play a huge role. Peer pressure, the desire for social acceptance, and the natural urge to experiment are powerful motivators. Some teens also turn to substances to self-medicate for stress, trauma, or pain, using them as a temporary escape. The isolation and anxiety from events like the COVID-19 pandemic also impacted substance use, leading to increased heavy use for some as a coping mechanism.
For a deeper dive into the fascinating world of the adolescent brain and behavior, we recommend exploring the wealth of scientific research on the adolescent brain and behavior.
How Substance Use Disrupts Brain Development
When substances enter the developing adolescent brain, they can cause lasting damage, a process known as neurotoxicity. The developing brain is far more vulnerable to the harmful effects of drugs and alcohol than an adult brain.
Substance use can lead to:
- Impaired Cognitive Function: Difficulties with attention, memory, and problem-solving that can impact school performance.
- Reduced Executive Function: Weakened impulse control and decision-making, making it hard to manage responsibilities.
- Increased Risk of Addiction: The brain’s sensitive reward system adapts quickly to substances, making it easier to develop a substance use disorder (SUD). The younger a teen starts, the greater the risk.
- Altered Brain Structure: Studies show changes in gray and white matter, which can have long-term impacts on brain function.
We encourage you to visit NIDA information on how substances affect the brain for more details on this critical topic.
Common Reasons Teens Give for Using Substances
Understanding why teens use substances is the first step toward prevention. It’s rarely one reason, but a complex mix of factors:
- To fit in: Peer pressure and the desire for social acceptance are powerful forces.
- To feel good: Substances activate the brain’s reward system, producing pleasure or relaxation.
- To feel better: Many teens use substances to cope with stress, anxiety, depression, or trauma (self-medication).
- To do better: Some mistakenly believe substances can improve academic or social performance.
- To experiment: Curiosity and a natural desire for novelty and risk-taking drive experimentation.
- Boredom: Some teens turn to substances to alleviate boredom or seek excitement.
The Spectrum of Adolescent Substance Abuse Health Risks
Now, let’s talk about the nitty-gritty: the actual health risks. The adolescent substance abuse health risks are wide-ranging, impacting everything from immediate safety to long-term well-being.
Short-Term Health Consequences
The immediate dangers of adolescent substance use can be severe and life-altering:
- Impaired Judgment: Clouded thinking leads to poor decisions with serious consequences.
- Accidents and Injuries: A leading cause of teen death, including motor vehicle crashes and falls.
- Risky Sexual Behavior: Lowered inhibitions can lead to unprotected sex, unwanted pregnancies, and STIs.
- Violence and Victimization: Drug use is associated with experiencing or perpetrating violence.
- Alcohol Poisoning: Binge drinking (consuming 4-5+ drinks quickly) is extremely dangerous and can be fatal.
- Drug Overdose: With fentanyl in the drug supply, even one use can be fatal. Overdose is a leading cause of death among adolescents.
- Poor Academic Performance: Substance use can cause memory problems and disinterest in school, leading to failing grades.
- School Absenteeism: Skipping school is a common consequence, increasing the risk of dropping out.
Understanding the Long-Term Adolescent Substance Abuse Health Risks
While the short-term consequences are alarming, the long-term adolescent substance abuse health risks are perhaps even more insidious:
- Substance Use Disorder (SUD): The most significant risk. Most adults with an SUD started using as teens; early initiation dramatically increases this likelihood.
- Chronic Health Diseases: Prolonged use contributes to liver damage, heart disease, respiratory issues, and cancer.
- Lasting Cognitive Impairment: Persistent problems with memory, learning, and attention can affect future education and careers.
- Higher Rates of Mental Illness: There’s a strong link between substance use and conditions like depression, anxiety, and psychosis.
- Increased Risk of Suicide: The combination of substance use and mental health issues lifts the risk of suicidal thoughts and attempts.
- Poor Functional Outcomes: Teens with SUDs often face lifelong challenges in education, employment, and relationships.
Specific Adolescent Substance Abuse Health Risks by Substance
Different substances carry different risks. Here’s a breakdown of some common substances and their specific adolescent substance abuse health risks:
| Substance | Primary Short-Term Health Risks | Primary Long-Term Health Risks |
|---|---|---|
| Alcohol | Impaired judgment, car crashes, fights, risky sexual activity, alcohol poisoning, blackouts. Binge drinking is particularly dangerous. | Alcohol use disorder (AUD), liver damage (cirrhosis), pancreatitis, heart problems, cancer, lasting cognitive deficits, memory impairment, and mental health conditions like depression and anxiety. |
| Nicotine/Vaping | Highly addictive, acute nicotine poisoning (nausea, seizures), lung irritation, increased heart rate/blood pressure, exposure to harmful chemicals. | Permanent brain changes affecting attention, learning, and impulse control. Increased risk of other substance use, chronic lung diseases, cardiovascular problems, and cancer. |
| Cannabis | Impaired memory, learning, and motor coordination; distorted perception; anxiety, paranoia, or psychosis (especially with high-potency strains). | Cannabis use disorder (CUD), lasting negative effects on cognitive function (attention, memory), increased risk of mental health conditions like anxiety, depression, and psychosis, and respiratory problems if smoked. |
| Opioids | Severe respiratory depression, unconsciousness, overdose (often fatal due to fentanyl), nausea, sedation, addiction. Injection use carries a high risk of HIV and other blood-borne diseases. | Opioid use disorder (OUD), chronic health issues, high risk of overdose death, infectious diseases (HIV, hepatitis) from injection use, and severe legal, financial, and social problems. |
| Other Illicit/Prescription Drugs | Varies widely but includes overdose, seizures, heart attack, psychosis, and impaired judgment. Includes cocaine, meth, ecstasy, and misused prescription stimulants (e.g., Adderall) or benzodiazepines (e.g., Xanax). | Varies widely but includes severe addiction, permanent brain and organ damage, chronic mental health conditions, neurological disorders, and severe legal, financial, and social dysfunction. |
Identifying Vulnerability: Risk Factors, Warning Signs, and Co-Occurring Conditions
Understanding the adolescent substance abuse health risks is crucial, but so is knowing who is most vulnerable and what signs to look for. Certain factors increase the likelihood of a problem, and recognizing warning signs can lead to timely intervention.
Key Risk Factors for Teen Substance Use
Risk factors are interconnected and can include:
- Family history of addiction: A teen with a close relative who has an SUD is 3-5 times more likely to develop one.
- Parental attitudes and monitoring: Permissive attitudes or a lack of supervision increase risk.
- Peer substance use: Association with substance-using peers is a strong predictor.
- Mental health conditions: ADHD, depression, and anxiety significantly increase risk, as teens may use substances to self-medicate.
- History of trauma or abuse: Adverse childhood experiences are strong predictors of using substances to cope.
- Early initiation of use: Starting substance use before age 14 dramatically increases the risk of developing an SUD.
- School and community environment: Lack of school connectedness, low achievement, and easy access to substances contribute to risk.
Signs and Symptoms of a Potential Problem
Many warning signs can mimic normal teen behavior, but a cluster of these signs, especially if they represent a change, warrants attention:
- Social and behavioral changes: Sudden changes in friends, secrecy, breaking rules, or loss of interest in hobbies and school.
- Mood and personality shifts: Increased irritability, mood swings, anxiety, paranoia, aggression, or lack of motivation.
- Changes in daily habits: Significant shifts in eating or sleeping patterns, or a decline in personal hygiene.
- Financial issues: Unexplained need for money, stealing money or valuables.
- Physical signs: Red or glazed eyes, persistent cough, fatigue, sudden weight changes, or finding drugs or paraphernalia.
If you observe several of these signs, it’s time to seek professional guidance.
The Link Between Substance Use and Mental Health
The relationship between substance use and mental health is often a “dual diagnosis” or “co-occurring disorder.” The two are so intertwined that a majority of adolescents with SUDs are also diagnosed with at least one other mental disorder. Mental health issues can lead to substance use (self-medication), and substance use can worsen or trigger mental health problems, creating a vicious cycle.
Common co-occurring conditions include:
- Depression and Anxiety: Teens may use substances for temporary relief, but use often worsens these conditions long-term.
- ADHD: Those with ADHD are at a higher risk for developing an SUD, sometimes using substances to self-medicate symptoms.
- Psychosis: High-potency cannabis use in adolescence is linked to an increased risk of psychotic disorders.
- Trauma-related disorders: Substance use is a common coping mechanism for symptoms of PTSD.
This complex interplay requires integrated treatment that addresses both conditions simultaneously. For more information, explore SAMHSA resources on co-occurring disorders.
Disparities in Substance Use and Consequences
Not all adolescents experience substance use or its consequences equally. Factors like gender, race, ethnicity, and sexual orientation play a significant role.
- Gender Differences: While males historically had higher rates of use, this gap is closing. For some substances like alcohol, adolescent females now report higher rates of use and binge drinking.
- Racial and Ethnic Disparities: While White youth may report higher rates of some substance use, youth of color often face harsher consequences. Black youth, for example, are disproportionately represented in juvenile drug cases, leading to criminalization rather than treatment.
- Access to Treatment: Disparities in access to quality care exist based on socioeconomic status, location, and the cultural competency of services.
- LGBTQ+ Youth: High school students who identify as lesbian, gay, or bisexual are almost twice as likely to use illicit drugs, often due to social stigma, discrimination, and lack of support.
Building Resilience: Prevention, Screening, and Finding Treatment
Understanding the adolescent substance abuse health risks is crucial, but what’s even more important is what we can do about it. Building resilience, fostering open communication, and knowing how to seek help are powerful tools for protecting teens.
The Parent’s Role: Prevention and Open Communication
Parents are the most influential factor in a teen’s life. Your role in preventing substance use is paramount.
- Set clear rules and consequences: Teens need structure. Clearly communicate your expectations about substance use and be consistent.
- Monitor your teen’s activities: Knowing where your teen is and who they are with is a key protective factor. This shows you are engaged and care.
- Build a strong bond: A supportive relationship is a powerful buffer. Spend quality time together, listen, and show interest in their lives.
- Talk about the risks: Have open, regular conversations about the dangers of drugs and alcohol, using facts, not scare tactics. Start these talks early.
- Model healthy behavior: Be a positive role model with your own choices regarding alcohol and medications. Secure prescription drugs and dispose of them properly.
The Substance Abuse and Mental Health Services Administration (SAMHSA) offers excellent resources through their SAMHSA’s “Talk. They Hear You.” campaign resources to help parents with these conversations.
Screening and Early Intervention
Don’t wait for a crisis. Early identification and intervention can drastically alter a teen’s future.
- Importance of screening: Routine screening for substance use during annual check-ups is a best practice. Pediatricians can use validated tools like the CRAFFT questionnaire to identify risk early.
- Role of professionals: Pediatricians and school counselors are the first line of defense. They can conduct screenings, provide brief interventions, and refer to specialists if needed.
- Trust your instincts: If you see the warning signs discussed earlier, reach out for help. Early intervention is key to preventing casual use from becoming a disorder.
Evidence-Based Treatment Options for Teens
If a teen is struggling with a substance use disorder, effective, evidence-based treatment is available. Treatment should be custom to the adolescent’s needs and should involve the family.
- Behavioral therapies: These are the cornerstone of treatment. Cognitive Behavioral Therapy (CBT) helps change negative thought patterns, while Multidimensional Family Therapy (MDFT) addresses family, peer, and community factors.
- Family-based therapy: Therapies that involve caregivers are highly effective. They improve communication and equip parents to support their teen’s recovery.
- Motivational interviewing: This counseling style helps teens find their own motivation to change their substance use behaviors.
- Pharmacotherapy (medications): Medications can be an important part of treatment, especially for opioid use disorder (e.g., buprenorphine for ages 16+) and nicotine addiction.
- Levels of care: Options range from outpatient counseling to residential treatment. It is vital that adolescents are treated in programs specifically designed for them, not alongside adults.
Finding the right support can feel overwhelming, but you don’t have to do it alone. We offer confidential guidance and can help you explore treatment options, including specialized adolescent programs in cities like Las Vegas, Reno, and Henderson, Nevada. For a confidential assessment and to find the right level of care for your loved one, call Drug Rehab Headquarters at 866-720-3784.
Conclusion
The adolescent substance abuse health risks are a serious concern for families and communities. We’ve seen how the unique developmental stage of adolescence, with its maturing brain and heightened vulnerability, can pave the way for experimentation to escalate into significant problems. From immediate dangers like accidents and overdose to long-term consequences like chronic illness, cognitive impairment, and severe mental health conditions, the stakes are incredibly high.
But there is hope. We firmly believe that early intervention is key to better outcomes. Parents are the first line of defense, equipped with the power of open communication, consistent monitoring, and modeling healthy behaviors. By understanding the risk factors, recognizing the warning signs, and knowing that effective, evidence-based treatment options exist, we can empower our teens to make healthier choices and build resilient futures.
If you or a loved one needs help understanding these risks or finding support, Drug Rehab Headquarters is here for you. We can connect you with resources and treatment options custom to adolescent needs. Don’t let uncertainty or fear prevent you from taking action. Call us today at 866-720-3784 for a free, confidential consultation.


